Woolcock Centre for Lung Cancer Research

Lung Cancer Research
Despite recent improvements in treatment, lung cancer remains the leading cause of cancer-related mortality in Australia with almost 9,000 deaths each year. If discovered early, lung cancers can be removed by surgery, but often the tumour is discovered too late and the only options available are systemic therapy or radiotherapy.
Immunotherapy has been recently introduced to the treatment of advanced lung cancer and involves boosting the body’s own immune system to attack the tumour. A type of immunotherapy is also in routine clinical use for asthma that is caused by an allergic reaction. In lung cancer, treatment with immune checkpoint inhibitor drugs is promising and works very well in a small subset of patients. The problem is that it still does not work for the majority of lung cancer patients and the tests used to select the patients for this therapy needs further refinement.
Project 1: Role of microbiome in lung diseases and immunotherapy
Researchers: Professor Maija Kohonen-Corish, Dr Anna McLean, Dr Steven Kao, Professor Wendy Cooper
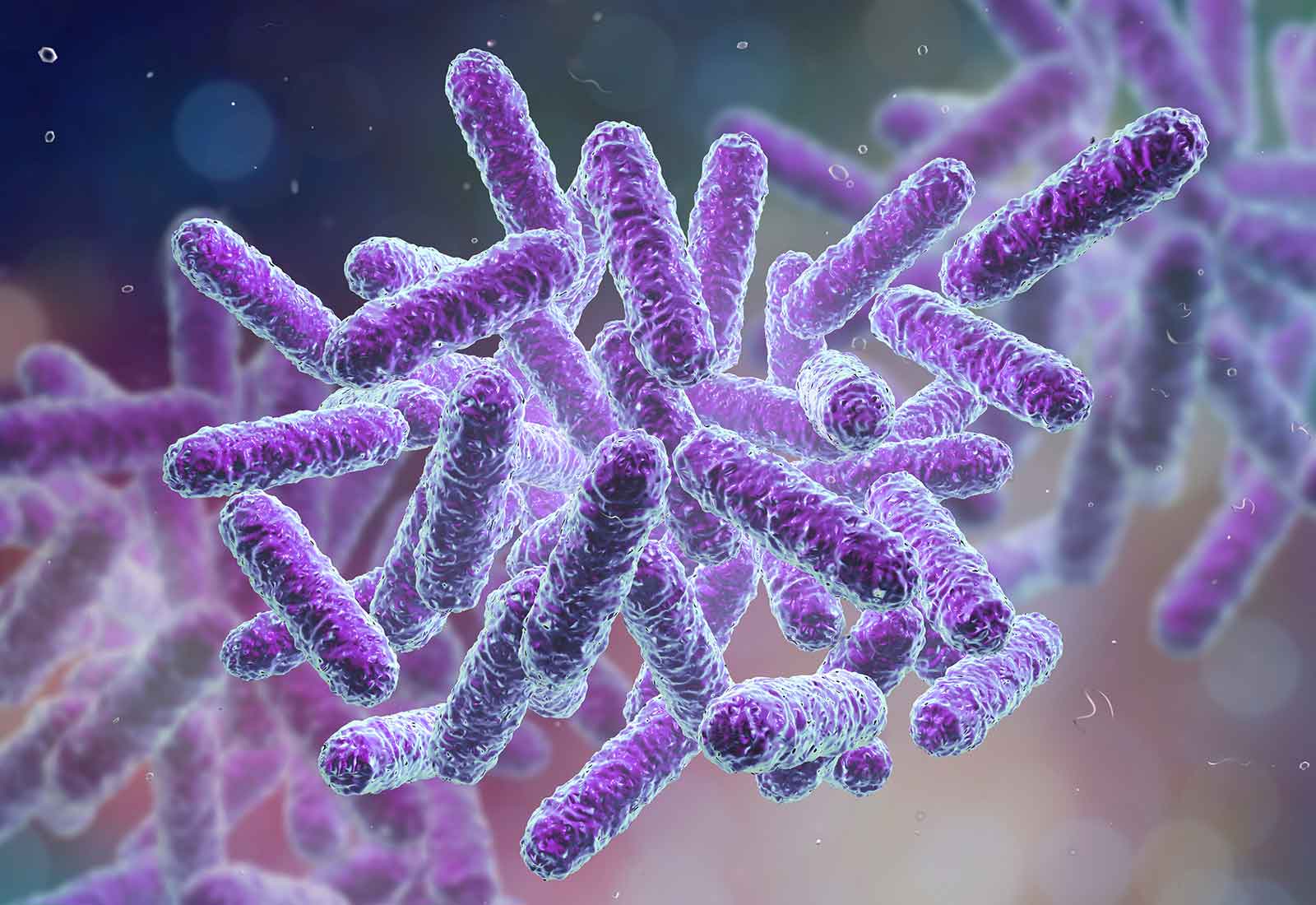
Very important evidence is emerging that the naturally occurring microbes in the gastrointestinal tract (gut microbiome) can interact with the body’s immune system to influence the efficacy of immunotherapy. Dysbiosis (a microbial imbalance or maladaptation) in the gut lowers the body’s immune defences. This has important implications for immunotherapy. It has been shown that dysbiosis can prevent immunotherapy from acting on its target, the tumour in the lung and other distant organs. Dysbiosis can be caused by diverse factors such as antibiotics, poor diet or alcohol misuse. Conversely, good bacteria in the gut can help the immune system attack the tumour.
This long-term project is conducted in collaboration with clinicians and researchers at Royal Prince Alfred, St George and Sutherland Hospitals, Microbiome Research Centre UNSW and Chris O’Brien Lifehouse. The aim is to determine how the human microbiome is altered in lung diseases and to identify the microbiome profiles that increase the efficacy of immunotherapy or are associated with resistance.
The findings of this research could have a major impact on the development of suitable interventions/supplements/adjunct therapy such as medical probiotics or inhalers, which will optimise the efficacy of immunotherapy for patients with lung cancer.

Project 2. Development of new biomarker testing to optimise immunotherapy
Researchers: Professor Maija Kohonen-Corish, Professor Brian Oliver, Dr Anna McLean, Dr Zeenat Jahan, Hannah Parker, Dr Steven Kao, Professor Wendy Cooper
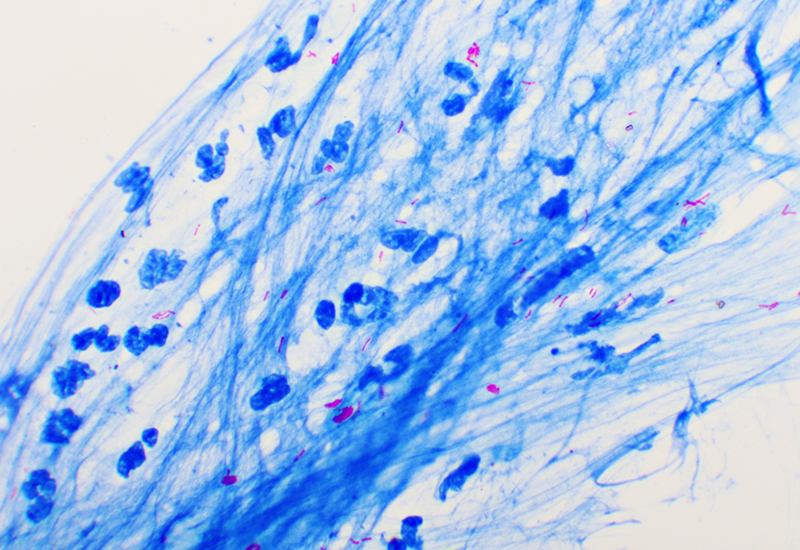
Immune checkpoint inhibitors (a type of immunotherapy) have shown promise in the treatment of a subset of lung cancer patients. One of the proteins that is an indicator of immunotherapy responsiveness of the tumour is PD-L1, a naturally occurring protein, which is now routinely assessed to help the physicians decide what kind of therapy is most suitable for the patient with advanced cancer. However, this is not an ideal biomarker and a significant number of patients with PD-L1-negative tumours also respond to immune checkpoint inhibitor drugs.
The aim of this research is to find better biomarkers for immune checkpoint inhibitor therapy by investigating other tumour proteins, DNA markers or microbiome profiling as alternatives for PD-L1 testing.
This project will potentially lead to the development of new predictive tests for response to immunotherapy in patients with lung cancer.
Inflammation and Cancer

PROJECT 3: DETERMINE HOW CHRONIC INFLAMMATION LEADS TO CANCER
Researchers: Dr Zeenat Jahan, Dr Hojabr Kakavand, Professor Maija Kohonen-Corish
It is increasingly recognised that one of the major questions in biomedical research is the role of inflammation in different diseases and the problem it poses for treatment. Chronic inflammation is a well-known risk factor for many types of cancer, such as colon, liver, pancreatic and lung cancer.
For example, long standing chronic colitis predisposes to colon cancer but inflammation also plays a role in sporadic colon cancers. In the lung, chronic obstructive pulmonary disease and emphysema predispose to cancer and it has been suggested that the inflammation found in asthma may also be a cofactor in lung cancer.
Our work aims to determine how inflammation leads to the development of cancer in individuals with inflammatory bowel disease (IBD), particularly in chronic colitis. By studying tumour tissue obtained from patients, we initially showed that a high percentage of early tumours in the bowel, including in IBD, do not express a gene called ‘MCC’. Subsequently the significance of this finding was determined and it was shown that the MCC gene is turned off (silenced) by cancer cells to help them multiply and spread.
A new MCC knockout mouse strain was developed that further helped understand the role of MCC silencing in cancer and allow us to study the very early stages of cancer development. The analysis revealed that the MCC knockout mice have a defect of DNA repair that is responsible for the increased frequency of cancer. DNA repair is an essential ‘housekeeping’ mechanism that is required to keep cells healthy. These mice are currently used to analyse a model of COPD in the development of lung cancer.
We continue to establish how these complex cellular pathways and mechanisms operate, in order to improve cancer therapies. We now know that MCC silencing in the tumour can also be beneficial for the patient because it makes the tumour more responsive to certain drugs. We are currently testing new combination of drugs in cultured cancer cells. Some of these drugs are already approved for use in the treatment of patients but our work will potentially provide a new biomarker to help optimise their use.
Therefore, our work can lead to rapid translation and better targeting of current cancer therapies. Ultimately, understanding these molecular mechanisms and processes may lead to new ways to treat or prevent all types of inflammation-associated cancer.