Asthma
Information for general practitioners and healthcare professionals
Many Australians are prescribed doses of inhaled corticosteroids that are higher than necessary to control their asthma. Prescribing unnecessarily high preventer doses increases the patient’s risk of adverse effects and may also increase the patient’s out-of-pocket costs.
Asthma guidelines recommend considering a step-down of preventer treatment after asthma has been well controlled for two to three months in adults and for six months in children. The step-down process should be individualised for each patient.
This page has information to help GPs and healthcare professionals plan and manage their patient's step-down. The advice here is founded on world-leading research about what works best for people with well-controlled asthma. If you have any questions or suggestions, please email the research team at helen.reddel@sydney.edu.au.
Step-down at a glance
- Use shared decision-making
- Timing is important
- Assess the patient’s risk factors
- Record the patient’s baseline asthma status
- Make small dose adjustments gradually
- Self-monitoring by the patient is important
- Make sure the patient has a written asthma action plan
- Review after stepping down
- Do not completely stop inhaled corticosteroids
For further information, see
- How to step down asthma preventer treatment in patients with well-controlled asthma – more is not always better, an article we published in the August 2022 issue of Australian Prescriber
- Australian Asthma Handbook
Which patients should be considered for a step-down?
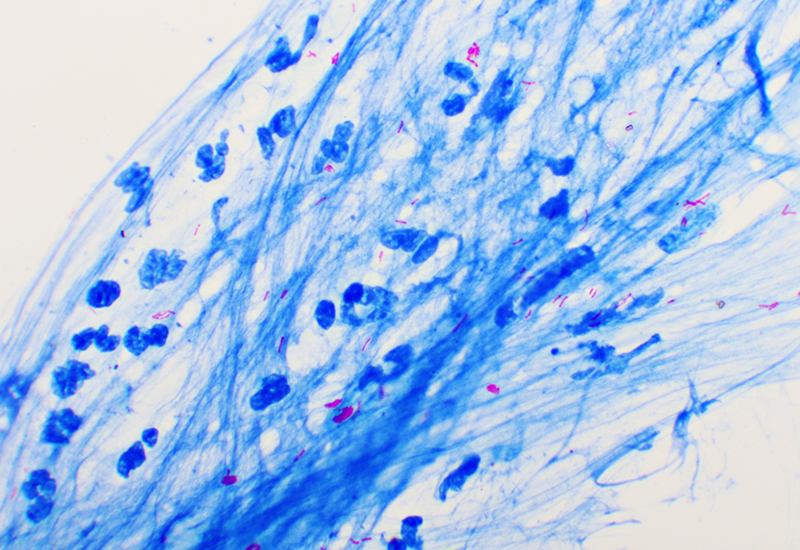
Evidence shows that preventer treatment can be stepped down safely. Systematic reviews of studies in properly selected patients found no overall increase in the risk of exacerbations. However, the dose of ICS that will keep asthma well controlled varies between patients, so consider each step-down as a treatment trial and monitor the patient closely afterwards.
All patients should have a written asthma action plan before starting a step-down. To assess symptom control, use a tool such as the Asthma Control Test. This evaluates symptoms, reliever use and perceived control over four weeks. The Woolcock's Peak Flow Chart makes it easy to detect exacerbations and gradual changes.
Keep in touch
Enter your details below and we'll send you email updates with other great resources for GPs and healthcare professionals. Please be assured we keep your information private. Read our privacy policies